- Chemoembolisation:
- Radioembolisation:
- Ablation Techniques:
- Pre- Operative Embolisation:
Treatments for cancers are a rapidly developing field, with marked advancements in Surgery, Chemotherapy and in Interventional Radiological techniques. Interventional Radiological techniques which initially used to be only palliative in nature, now can also be applied as a complementary to surgery, superior palliation and in few cases as a surgical alternative.
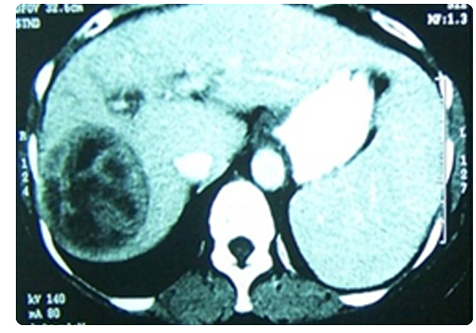
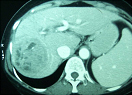
This has been a tried and tested method for Hepatocellular carcinomas (HCC), cholangiocarcinomas and in selected cases of colorectal metastasis. In this technique we go superselectively into the vessels supplying the liver lesions, and infuse chemotherapy drugs with a carrier (Lipiodol) and then reduce the vascularity with embolising agents. This technique allows the chemotherapy drug to act within the tumour, with a high concentration of the drug acting on the tumour specifically. This reduces the systemic side effects of the chemotherapy drug. With the advent of DC beads, the efficacy of chemoembolisation has greatly improved.
With advancement of catheter techniques, chemotherapy drugs and techniques the results of chemoembolisation are markedly improving. Multiple sittings are possible safely.
This exciting technique has been introduced over the last decade, which initially started for HCC and now has progressed to other hepatic lesions, such as colorectal metastasis, neuroendocrine metastasis, breast metastasis, etc.
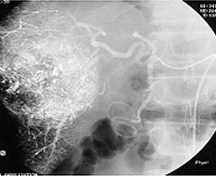
Here a beta radiating agent Yttrium 90, is coated with microspheres and is injected transarterially, superselectively into the tumour. This agent penetrates 3-5mm, thereby safely irradiating only the tumour. In this technique, detailed planning is required for the procedure and is to be performed only by experienced operators. It is a multistep procedure, which involves accurate volumetry, angiographic anatomical planning, shunt calculation with Tec 90, dose calculation,embolisation of the intestinal branches to prevent non-target embolisation, and final injection of the calculated dose superselectively into the tumour.
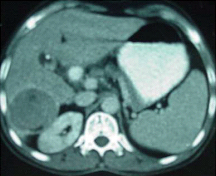
 Opted for Yttrium 90. Injection of Y 90
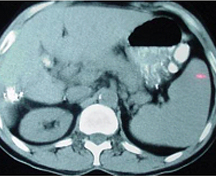
Opted for Yttrium 90. Injection of Y 90 2 months, post yttrium 90 injection, showed no activity within the lesion
2 months, post yttrium 90 injection, showed no activity within the lesionThis procedure has very few side effects, if done correctly, with very promising results. It is the treatment of choice in HCC palliation and with excellent results for liver metastasis. It can also be used in cases, where chemoembolisation is contraindicated- such as portal vein thrombosis, where radioembolisation can be used safely.
Chemoembolisation and radioembolisation can also shrink the tumour, making them suitable for surgical resection.
We have been pioneers in this technique in the country, with the largest experience with Yttrium 90. The protocol established by us in, conjunction with the nuclear medicine department, oncology and surgical oncology team, has helped us achieve results at par with international standards.
Ablation techniques are very promising for various tumours, with results equivalent to the gold standard, surgery. Various tumours such as HCC, bone tumours (osteoid osteoma,etc), renal tumours, lung tumours and breast tumours, which are inoperable, can be successfully treated by ablative techniques. The results are promising, offering a longer life span, better quality of life, pain relief and in some cases regression of the lesions.Various techniques are available, alcohol ablation for small (< 3cms) liver tumours.
Radiofrequency ablation (RFA); a technique which involves the use of thermal energy, to kill the tumour cells. RFA is performed by using a needle to transmit heat and burn the tumour, rendering it inactive. We perform it, extrapolating the surgical technique, of ablating a 1cm normal tissue.
Various tumours can be treated with RFA: HCC, liver metastasis, renal tumours, lung tumours, bony tumours and recent applications in the breast.

Embolisation is a well established interventional radiology technique that uses small solid particles or liquids to block the flow of blood. Certain tumours are very vascular and have the potential to bleed profusely during surgery; hence pre-operative embolisation can reduce the vascularity of the lesions, making them amenable to a safe resection.
We have used this technique successfully in liver tumours, renal carcinomas/angiomyolipomas, bone tumours (ABC, GCT, sarcomas), spinal tumours and in certain head and neck tumours (JNAF)
Portal vein embolisation is a well established technique, whereby the portal vein of an affected liver lobe is embolised, so as to promote hypertrophy of the normal liver lobe, enabling a successful therapeutic surgery.
Biliary drainages and Stentings, CT/USG guided therapeutic procedures, Percutaneous Nephorstomies and Antegrade drainages are routinely performed by us for various causes.